Introduction
Pregnant women often experience episodes of mild to moderate abdominal or pelvic pain throughout their pregnancy due to the numerous physiological and anatomical changes their bodies undergo.
Although most causes of abdominal pain during pregnancy are benign and expected, some may signal a more serious issue. In addition to pregnancy-related complications such as ectopic pregnancy, miscarriage, or problems with the uterus and placenta, pregnant women can also experience abdominal illnesses common to anyone, such as appendicitis, cholecystitis, pancreatitis, urinary tract infections, gastroenteritis, and so on.
Therefore, if you are pregnant, it is important to educate yourself about the most common causes of abdominal pain during pregnancy so that you can recognize symptoms that might indicate potentially serious issues.
Abdominal pain during pregnancy caused by the pregnancy itself
Episodes of abdominal or pelvic pain typically arise during the first few months of pregnancy and can last until childbirth. Pregnancy’s “normal” abdominal pain is usually not constant, but can occur quite frequently throughout the nine months.
The causes and characteristics of abdominal pain change as the pregnancy progresses. Hormonal changes, alterations in abdominal and pelvic anatomy, uterus growth, uterine contractions, fetal movement, compression of abdominal organs, and changes in pelvic ligaments are common causes of “normal” pregnancy pains.
There are also pregnancy pains that are not considered normal, meaning they are caused by complications during pregnancy. These pains, which may indicate a more serious issue, need to be identified early so that the pregnant woman can seek prompt obstetric care, minimizing the risk of complications.
Below, we explain the causes of abdominal pain during pregnancy, whether normal or abnormal, according to the trimester of gestation.
Common causes of abdominal pain in the first trimester
“Normal” pains in the first trimester
In the first few months of pregnancy, abdominal pain is often caused by hormonal changes that interfere with the normal functioning of the intestines. Excess gas, bloating, and constipation are some of the issues that may lead to pregnant women experiencing abdominal discomfort as early as the first trimester (read: 25 early pregnancy symptoms).
Generally, these pains are mild and temporary. Any intense, persistent abdominal pain, or pain accompanied by symptoms such as vaginal bleeding, purulent vaginal discharge, fever, profuse diarrhea, bloody diarrhea, hypotension, exhaustion, or vomiting* should be evaluated by your obstetrician.
*Note: Nausea and vomiting are common in the first trimester of pregnancy, but they usually are not associated with abdominal pain, fever, or diarrhea.
In the first trimester of pregnancy, the two main causes of abdominal pain due to pregnancy complications are ectopic pregnancy and miscarriage.
Ectopic pregnancy
Ectopic pregnancy refers to any pregnancy that develops outside the uterus, such as in the fallopian tube.
Obviously, any part of a woman’s body besides the uterus is not equipped to sustain a pregnancy, leading to serious complications as the fetus grows. Ectopic pregnancy is a medical emergency.
Symptoms of ectopic pregnancy often appear starting from the 6th week of pregnancy. The most common are:
- Moderate to intense unilateral abdominal pain (on the side where the embryo has implanted), typically in the lower abdomen.
- Abdominal muscle stiffness.
- Vaginal bleeding.
- Pain during bowel movements.
- Presence of a palpable mass in the groin area (in case of ectopic pregnancy in one of the fallopian tubes).
- Nausea and vomiting.
The diagnosis is usually made through ultrasound, which can show that the embryo is not located inside the uterus.
Miscarriage
Miscarriage (also called a spontaneous abortion) refers to any spontaneous and unexpected interruption of pregnancy that occurs before the 20th week of gestation. Pregnancy interruptions after the 20th week are called preterm births.
Miscarriage is one of the causes of abdominal pain in the first trimester of pregnancy. Most spontaneous abortions occur within the first 13 weeks of pregnancy.
Signs and symptoms of miscarriage include:
- Moderate cramp-like pain in the midline of the abdomen.
- Pelvic pain.
- Light to moderate vaginal bleeding.
- Uterine contractions that occur every 5 to 20 minutes. The cramps may resemble uterine contractions during menstruation.
Gynecological examination and ultrasound are generally used to confirm an ongoing miscarriage.
Septic abortion
Septic abortion is not exactly a cause of abdominal pain that occurs during pregnancy, but rather shortly after an abortion.
Septic abortion refers to any abortion, spontaneous or induced, that is complicated by uterine infection. It is generally the result of an abortion or uterine evacuation performed without appropriate surgical equipment, sterile preparation, or trained healthcare professionals. It is a common complication in “clandestine abortions.”
Septic abortion is a clinical diagnosis made in pregnant women who present with signs and symptoms of uterine infection, including abdominal or pelvic pain, purulent vaginal discharge, vaginal bleeding, or fever following the loss or interruption of pregnancy.
“Normal” pains from the second trimester onward
By 12 weeks of pregnancy, the uterus has grown enough to become an intra-abdominal organ (previously, it was located only in the pelvis). Therefore, in addition to all the causes of “normal” abdominal pain from the first trimester, pregnant women now also experience aches and discomforts caused by the compression of abdominal organs by the uterus and the progressive increase in weight that the pelvis must bear.
Toward the end of pregnancy, the baby’s natural movements and “kicks” can cause temporary pain or discomfort in the pelvic region or abdomen.
Braxton Hicks contractions
Braxton Hicks contractions are non-expulsive uterine contractions that usually appear starting from the 2nd trimester of pregnancy (in some women, they may occur at the end of the first trimester) and serve as “practice” for the uterus.
These contractions are harmless; they tend to be short, with irregular intervals and low frequency. Braxton Hicks contractions do not increase the risk of preterm birth and cause more discomfort than actual pain.
Generally, changing positions and resting are enough to make them disappear. Dehydration can trigger these contractions, which is why most doctors recommend patients drink more water if they occur frequently.
To learn more about Braxton Hicks contractions, read: What are Braxton Hicks Contractions (AKA False Labor)?
Round ligament pain
The round ligaments are like two cords on each side of the uterus. Each one is about 10 centimeters (4 in) long. The round ligaments connect the uterus to the pelvis and help keep the uterus in place.
The round ligaments become increasingly stretched and strained as the uterus grows and becomes heavier.
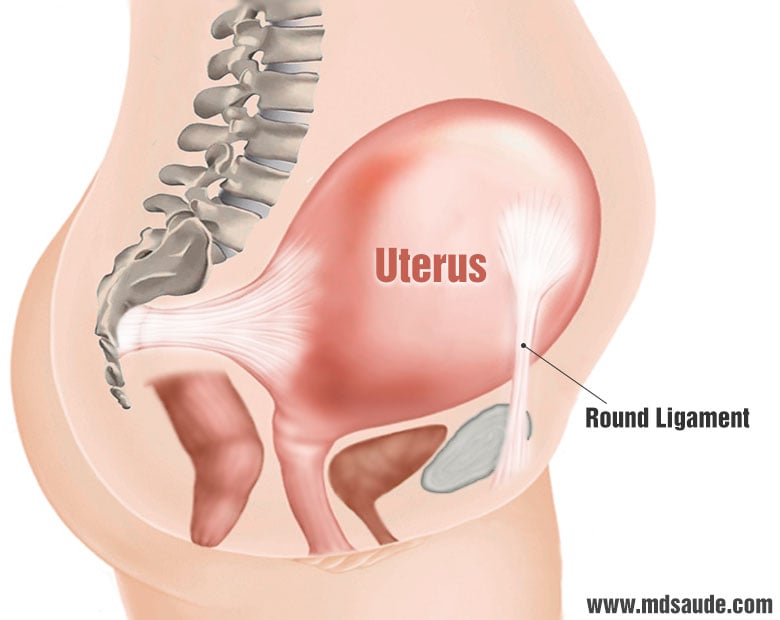
This stretching usually begins in the second trimester and increases as pregnancy progresses. The pain it causes is often a sharp sensation in the pelvis or lower abdomen that occurs when the pregnant woman changes position. Getting out of bed, coughing, standing up from a chair, and getting out of a car are some situations that can trigger round ligament pain.
The pain can also occur continuously after a particularly active day when the pregnant woman has walked a lot or exerted more effort than she should have.
Abdominal pain related to complications from the second trimester of pregnancy
As pregnancy progresses, the number of possible gestational complications also increases, especially after the 20th week. We will briefly discuss some of these complications that are frequently accompanied by abdominal pain.
Uterine incarceration
The term incarcerated gravid uterus refers to a pregnant uterus that becomes trapped between the sacral promontory and the pubic symphysis (bones located at the back and in front of the pelvis, respectively) as it grows.
When the uterus becomes incarcerated, it grows in the pelvis rather than towards the abdominal cavity, causing compression of the urethra, bladder, and rectum.
Typical symptoms of uterine incarceration include:
- Difficulty urinating or defecating.
- Sensation of incomplete emptying.
- Urinary retention.
- Abdominal pain.
- The absence of adequate growth of the uterus in the abdominal region.
Labor
Any birth after the 37th week of pregnancy is considered normal and classified as a full-term pregnancy. On the other hand, preterm birth is considered when it occurs before the 37th week of gestation. The more premature the birth, the less time the baby will have had for intrauterine development, thus increasing the risk of complications for the newborn.
As in miscarriages, labor also manifests with abdominal pain. The most common symptoms are:
- Frequent and rhythmic uterine contractions that intensify over time.
- Mild vaginal bleeding.
- Rupture of membranes.
- A feeling of pressure in the pelvic region.
The pregnant woman should contact her obstetrician immediately at the slightest sign of preterm labor. A gynecological examination can identify whether the uterus is indeed in the process of expelling the fetus.
Placental abruption
Placental abruption (PA) occurs when the placenta partially or completely detaches from the uterine wall. This is a serious pregnancy complication because the detachment prevents the placenta from continuing to receive blood from the uterus, endangering the life of the fetus.
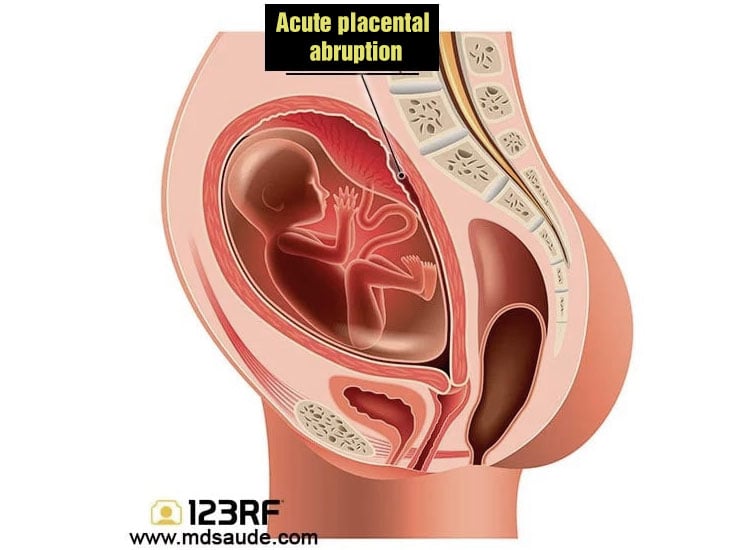
Placental abruption is more common in the 3rd trimester of pregnancy, but can occur from the 20th week of gestation.
The most common symptoms of placental abruption are:
- Vaginal bleeding, which can be heavy or mild.
- Intense abdominal and lower back pain.
- Uterine contractions.
- Low blood pressure (in cases of massive bleeding).
PA is also a medical emergency; labor induction is usually the treatment of choice.
Preeclampsia and eclampsia
Preeclampsia is a syndrome characterized by the onset of high blood pressure and proteinuria (protein loss in the urine) after 20 weeks of gestation. In more severe cases, the liver may also be involved.
Abdominal pain, facial swelling, swelling of hands and legs, headache, blurred vision, nausea, and vomiting are the most common symptoms. When a pregnant woman with preeclampsia develops a seizure, the condition is called eclampsia.
Intrahepatic cholestasis of pregnancy
Intrahepatic cholestasis of pregnancy, also known as obstetric cholestasis, is a complication that occurs in the third trimester of pregnancy and affects about 1% of pregnant women.
Cholestasis is characterized by increased levels of bilirubin in the blood, caused by the obstruction of the liver’s bile ducts.
The main symptom of pregnancy cholestasis is intense itching, mainly on the palms of the hands and soles of the feet, which usually appears from the 30th week of pregnancy.
In about 25% of pregnant women, one to four weeks after the onset of itching, other symptoms may appear, such as jaundice (yellowish skin), loss of appetite, nausea, abdominal pain in the upper right quadrant of the abdomen, pale stools, fatty stools, dark urine, and fatigue.
Intra-amniotic infection
Intra-amniotic infection or clinical chorioamnionitis is an intrauterine infection that involves the membranes surrounding the fetus (chorion or amnion), the amniotic fluid, or the placenta.
Intrauterine infection usually arises when bacteria migrate from the vaginal region through the cervical canal into the uterus. This situation is more common in patients who have a premature rupture of membranes or take many hours from rupture to delivery (usually more than 18 hours apart).
Signs and symptoms of intra-amniotic infection include fever, abdominal pain, uterine tenderness, leukocytosis, maternal and fetal tachycardia, and uterine contractions.
Other causes
Other less common pregnancy complications that occur from the second trimester and can cause abdominal pain include:
- Uterine rupture.
- Spontaneous hemoperitoneum.
- Uterine torsion.
- Adnexal torsion (twisting of the ovaries or fallopian tube).
Causes of abdominal pain not related to pregnancy
Like any individual, pregnant women can also have abdominal illnesses not specific to pregnancy, such as appendicitis, cholecystitis, gastroenteritis, or kidney stones.
Diagnosing these problems is typically more complex in pregnant women due to the numerous anatomical changes their abdominal region undergoes. Even the location of the pain can be atypical.
Among the dozens of abdominal complications that can occur during pregnancy but are not directly related to pregnancy, one stands out: urinary tract infection.
Urinary tract infection in pregnancy
Cystitis, the name given to bladder infection, is a common issue during pregnancy. It can occur at any time during pregnancy. Its most common symptoms include:
- Pain or burning during urination.
- Frequent urge to urinate.
- Difficulty holding urine.
- Desire to urinate even with an empty bladder.
- Pain or heaviness in the bladder.
- Blood in the urine.
References
- Approach to acute abdominal pain in pregnant and postpartum women – UpToDate.
- Causes of abdominal pain in adults – UpToDate.
- Baby Belly Aches: 15 Causes of Abdominal Pain in Pregnancy – Medscape.
- Acute abdominal emergencies associated with pregnancy – Clinical obstetrics and gynecology.
- Surgical gastrointestinal disorders during pregnancy – American journal of surgery.
- Gastrointestinal Conditions during Pregnancy – Clinics in colon and rectal surgery.
- Evaluation of abdominal pain in pregnancy – BJM.
Author(s)
Médico graduado pela Universidade Federal do Rio de Janeiro (UFRJ), com títulos de especialista em Medicina Interna e Nefrologia pela Universidade Estadual do Rio de Janeiro (UERJ), Sociedade Brasileira de Nefrologia (SBN), Universidade do Porto e pelo Colégio de Especialidade de Nefrologia de Portugal.








