What is shingles?
Shingles, also known as herpes zoster, is an infectious disease caused by the Varicella-Zoster virus (VZV), the same virus that causes chickenpox (varicella).
Although caused by the same virus, shingles and chickenpox are different in terms of symptoms, epidemiology, and complications. While they share the same infectious agent, they are not the same disease.
Shingles is also not related to herpes labialis or genital herpes. The name herpes zoster suggests a similarity to herpes, and the virus family is the same: Herpesviridae. However, herpes zoster and oral or genital herpes are entirely different diseases.
How does shingles appear?
When we are exposed to the Varicella-Zoster virus for the first time, which usually occurs during childhood, we develop chickenpox, a disease characterized by fever and red rashes all over the body.
After one or two weeks of symptoms, our immune system creates antibodies, controls virus replication, and the disease disappears spontaneously.
The problem is that curing the symptoms does not necessarily mean curing the virus.
During the initial phase of chickenpox, the virus invades the nerve endings of the skin and migrates to some chains of ganglia located near the spinal cord and brain, thus managing to remain “hidden” from the immune system for periods that can last decades.
The patient is thus cured of chickenpox but remains infected with the Varicella-Zoster virus for the rest of their life.
In general, this is not an issue because every time the virus tries to come out of its “hiding place” in the nerve ganglia, our immune system, which now has specific antibodies against the Varicella-Zoster virus, manages to stop it.
The patient keeps the virus trapped, shows no symptoms, and cannot pass it on to others.
However, our battle against Varicella-Zoster depends on a robust immune system. The virus can wait decades for an immune-weakening event to multiply again.
When this happens, the reactivation of Varicella-Zoster does not cause a new chickenpox episode, but a different disease called shingles.
Symptoms
When the VZV reactivates, it takes the reverse route, traveling from the nerve back to the skin.

When the virus reaches the skin, it causes the typical lesions of herpes zoster: multiple reddish vesicles (blisters), which are restricted to a small area of the body, precisely the one that is innervated by the nerves that “hid” the virus.
The bumps on darker skin may have a pink, grayish, purple, or brown color, while on lighter skin they appear red or pink.
The way in which the shingles lesions are grouped, usually in a “stripe” and never extending beyond the midline of the body, is the most crucial characteristic for diagnosing the infection.
To understand why the shingles lesion behaves this way, you need to know a little about the anatomy of the spinal cord and its nerves. We will explain it in a simple way.
The spinal cord is connected to the brain, stands about 45 cm long, and lies inside the spine. It runs from the first cervical vertebra at the top of the neck to the second lumbar vertebra.
Several peripheral nerve plexuses run along the spinal cord throughout the body, which are responsible for innervating specific regions. Each region of the body that receives a branch of nerves from the medulla is called a dermatome.
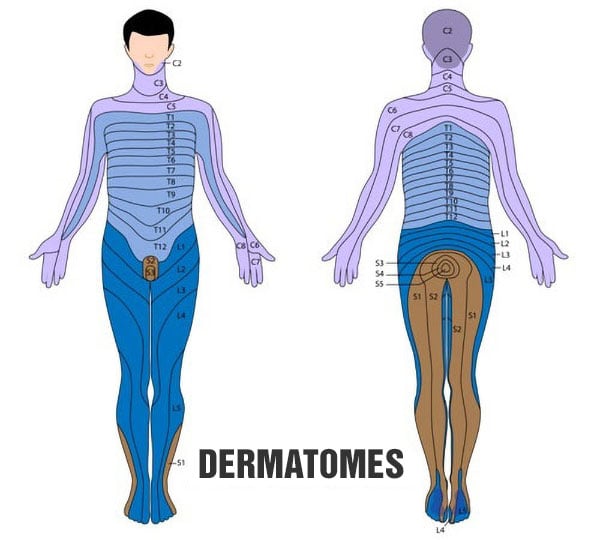
Each vertebra gives off a pair of nerves, each innervating one side of the body. The left and right nipple regions, for example, are innervated by a pair of nerves that originate at the 4th vertebra of the thoracic spine (T4). On the other hand, the navel area is innervated by nerves that arise at the 10th thoracic vertebra (T10).
Therefore, if the Varicella-Zoster virus is hidden in ganglia near the nerve root to the left of the T10 vertebra, for example, when reactivated, it will travel to the navel area and cause rashes in a strip of the abdomen that is to the left of the navel.

The photo above shows a shingles rash affecting the region innervated by T1 and T2. Note that the rash appears in a band-like pattern and stops precisely at the midline of the body, as the virus tends to affect only one of the nerves.
The dermatome affected by shingles usually has a burning or tingling sensation for one or two days before the lesions appear. General viral symptoms such as fever and malaise are also common.
When shingles appears, it usually starts as an excruciating, reddish rash, quickly developing into the typical vesicles (blisters). The thoracic, abdominal, and lumbar regions are the most affected.

New vesicles appear over 3 to 5 days, usually improving after 7 to 10 days when the blisters dry up and begin to scab over. The lesions and pain can take up to a month to disappear completely. In some cases, the zoster lesion can leave a scar.
Unlike chickenpox, which appears only once in a lifetime, shingles can recur whenever there is a drop in the patient’s immunity.
To see more pictures of shingles skin lesions, go to the link: Photos of shingles.
Complications
Post-herpetic neuralgia is a complication where pain persists at the affected site, even after the lesion has resolved for a long time. Though the infection disappears, the pain lingers.
In some cases, the pain of post-herpetic neuralgia is so intense and continuous that it can lead to depression and physical disability.
Usually, shingles is self-limiting and affects a small area of the body, usually only one dermatome. If new blisters are still appearing after 7 to 10 days or if the condition affects several dermatomes simultaneously, one should consider the possibility of a debilitating immune system disease, such as cancer or AIDS.
The reactivation of shingles on the face can be dangerous, especially if it affects the eye area, which can lead to loss of vision.
Ramsey Hunt syndrome is a facial paralysis that occurs when shingles affects the facial nerves. Labyrinthitis is also common in this syndrome.
How do you get shingles?
The patient with active shingles is contagious only to people who have never had chickenpox, i.e., those who have never been infected by the Varicella-Zoster virus.
If someone who has never had chickenpox comes into contact with someone who has mumps, they will develop chickenpox and not shingles. This is because chickenpox is always the first form of contamination by the virus.
The lesions are highly contagious, and the transmission of the virus usually occurs through hands infected by the lesions (it is enough to scratch or touch the lesion to risk contamination of the hands).
It is worth emphasizing that shingles itself is not transmissible. No one develops shingles without first having chickenpox.
If you currently have shingles but cannot remember having chickenpox as a child, it is possible that your case of chickenpox was so mild that it went unnoticed or was mistaken for another viral infection.
To get shingles, you need to have the Varicella-Zoster virus hiding in your nervous system. Having contact with someone with shingles will not make you have it too.
Individuals who have had chickenpox at any point in their lives, or have received the varicella vaccine, can interact with individuals who have shingles without any fear of contracting the illness. This is because they possess antibodies that can fight against the Varicella-Zoster virus.
Risk factors
As already mentioned, in order to have shingles, you must have had chickenpox at some point in your life. Up to 20% of patients with a history of chickenpox in childhood will have at least one episode of shingles, which usually appears after age 50. Among patients older than 85 years, this rate rises to more than 50%.
Shingles is a condition that occurs when the body’s immune system is weakened. Factors that increase the risk of developing shingles include:
- Age over 50 years.
- Physical or psychological stress.
- Sleep deprivation.
- Diabetes mellitus.
- Cancer
- Chemotherapy.
- Chronic diseases.
- Use of immunosuppressive drugs.
- HIV / AIDS.
Treatment
In most cases, shingles disappears spontaneously after a few days.
Treatment with oral antivirals such as Acyclovir, Valacyclovir, or Famciclovir is indicated to speed up the healing process. These antivirals are drugs that, if started within the first 72 hours of illness, reduce the severity, duration, and risk of complications of shingles.
The doses commonly used to treat shingles are as follows:
- Valacyclovir: 1000 mg three times a day for seven days.
- Famciclovir: 500 mg three times a day for seven days.
- Acyclovir: 800 mg five times a day for seven days.
If the illness has been present for over 72 hours, but new blisters continue to emerge, one may consider attempting antiviral therapy.
There is no evidence that topical antivirals, in cream or ointment form, are effective in shingles.
In some patients, the pain of shingles can be severe, and the use of analgesics is indicated. In some cases, the pain is so intense that opioids must be used to control it.
Since the pain is of neurological origin, antidepressant drugs such as Amitriptyline or Nortriptyline, or anticonvulsants, such as Gabapentin or Pregabalin, can also be used to relieve symptoms, especially in cases of post-herpetic neuralgia.
Vaccine against herpes zoster
In recent years, vaccination of children against chickenpox has been adopted in many countries and hypothesized to be effective against shingles as well.
The chickenpox and shingles vaccines are basically the same, but to be effective against shingles, the vaccine needs to be at least 14 times more potent than the chickenpox vaccine (i.e., have 14 times more viral particles).
Studies have revealed that the shingles vaccine is efficient in people over the age of 50 and can decrease the likelihood of experiencing shingles by as much as 70%.
Patients who have been vaccinated against shingles have a lower risk of developing complications even if they still end up getting the disease, compared to those who have not been immunized. This highlights the effectiveness of the vaccine in preventing severe consequences.
It is recommended to get immunized with the zoster vaccine for individuals over 50 years of age. This not only helps in preventing the disease but also reduces the risk of complications. Even if someone has had chickenpox or shingles before, they can still benefit from the vaccination.
Please note: the shingles vaccine, like any other vaccine, is used to prevent the disease, not to treat it.
FAQ
Is shingles contagious?
Yes, but only for people who have never had contact with the Varicella-Zoster virus. People who have never had chickenpox can become infected if they have contact with a patient with shingles. However, this person will have chickenpox and not shingles, which is a disease that appears only when the virus is reactivated.
Those who have had chickenpox before do not need to worry about possible infection, as the immune system is prepared to prevent new infections.
Is shingles dangerous?
Shingles is not usually dangerous for healthy individuals. However, it can cause significant pain and discomfort during the acute phase of the disease.
Anyone with shingles on the face, especially near the eyes, no matter how mild, should seek medical attention because of the risk of permanent eye damage.
One in five patients with shingles develops post-herpetic neuralgia, a permanent pain condition even after the skin lesions resolve.
Rarely, shingles can lead to pneumonia, hearing problems, brain inflammation (encephalitis), or death.
Can you have internal shingles (shingles without a rash)?
Yes. This condition is called zoster sine herpete.
Zoster sine herpete is one of the atypical clinical manifestations of shingles and derives from reactivation of the varicella-zoster virus in the cranial nerve, spinal nerve, viscera, or autonomic nerves.
Patients with zoster sine herpete present with neuralgia (pain of neurological origin), but do not manifest the typical skin lesions of shingles, which makes clinical diagnosis quite tricky.
Zoster sine herpete not only causes symptoms, such as neuropathic pain in the affected nerve, but also Bell’s palsy, Ramsay Hunt syndrome, post-herpetic neuralgia, and potentially fatal complications, such as encephalitis or stroke.
Is shingles an autoimmune disease?
No, shingles is an infectious disease that arises when there is some weakening of the immune system, but it does not have an autoimmune origin.
Can shingles have an emotional origin?
Experiencing psychological stress or trauma can potentially trigger shingles. This can include events such as losing a job, the passing of a family member, a highly stressful work environment, or insufficient sleep.
How long does shingles pain last?
In most patients, the pain lasts 2 – 4 weeks. In some patients, however, the pain may take up to 3 months to disappear completely. If, after 90 days, there is no improvement, the patient probably has post-herpetic neuralgia.
References
- Varicella and herpes zoster vaccines: WHO position paper, June 2014 – World Health Organization.
- Shingles (Herpes Zoster) – Centers for Disease Control and Prevention (CDC).
- Shingles (herpes zoster) – Public Health England.
- Epidemiology, clinical manifestations, and diagnosis of herpes zoster – UpToDate.
- Treatment of herpes zoster in the immunocompetent host – UpToDate.
- Vaccination for the prevention of shingles (herpes zoster) – UpToDate.
- Zoster sine herpete: a review – The Korean journal of pain.
Author(s)
Médico graduado pela Universidade Federal do Rio de Janeiro (UFRJ), com títulos de especialista em Medicina Interna e Nefrologia pela Universidade Estadual do Rio de Janeiro (UERJ), Sociedade Brasileira de Nefrologia (SBN), Universidade do Porto e pelo Colégio de Especialidade de Nefrologia de Portugal.








![Pictures: Syphilis – All stages [Warning: Strong Images]](https://www.mdsaude.com/wp-content/uploads/sifilis-imagem.jpg)